BRÜCKNER TEST (Fundus red reflex test)
Early detection of ocular disorders in children
The Brückner Test with the direct ophthalmoscope is a simple and useful examination to diagnose ametropia and abnormalities of the eye at an early stage to prevent irreversible amblyopia.
On this page HEINE provides you with information to the Brückner Test (often also referred to as red reflex test or transillumination test) and the use of a direct ophthalmoscope.
Background information to the Brückner Test
Childhood amblyopia is a frequent vision disorder with a prevalence of approx. 5 %.* Delayed recognition of an amblyopia in childhood may lead to permanent dysfunction of the eye or both eyes and correspondingly affect the development of a child.
Possible causes are:
- Ametropia
- Anisometropia (unequal refractive power)
- Myopia (nearsightedness)
- Hypermetropia (farsightedness)
- Astigmatism
- Manifest strabismus
- Dysplasia (e.g. congenital cataract or retinoblastoma)
With Brückner’s transillumination test cataract can be diagnosed in a simple, quick and highly sensitive manner. In addition, myopia (nearsightedness) and anisometropia (unequal refractive power) can be diagnosed with an examination at a distance. Changes on the posterior segments of the eye can also be detected.
Definition of amblyopia according to Ehrt
Amblyopia (weaksightedness) is defined as a reduction in the visual acuity of one or seldom both eyes – as a consequence of a disturbed development of vision. In more than 90 % of cases, common causes of amblyopia are strabismus, a refractive error (ametropia) or a combination of both. Rare causes are unilateral and bilateral congenital cataract or ptosis, development abnormalities of the anterior and posterior segment of the eye or temporary disturbances e.g. caused by injuries or eye bandages that were worn too long.
Weaksightedness describes therefore the neuronal deficit, which can only be corrected within the first few years of life, whereas ametropia describes the pure optical defect as cause of amblyopia which can be corrected at any time with glasses. Strabismus in children often leads to reduced acuity development of the deviated eye (amblyopia) but also to defects in stereo vision (binocular spatial vision).
Source: "Neues zur Amblyopie - Diagnostik und Therapie" Oliver Ehrt Kinderärztliche Praxis 83, 300 - 337 (2012) Nr. 6
Definition of amblyopia according to Gräf
Weaksightedness as cause of a disturbed development of vision, although the anatomical and physiological preconditions are met. The basic function disorder and the main symptoms for every amblyopia are reduced vision with crowding, of different intensity, which can only be detected when comparing neighbouring optotypes.
The most common causes of amblyopia are ametropia and manifest strabismus. Organic disorders of the eye and eye lids are rather seldom, but are very serious if they do occur. The prevalence of amblyopia in Germany is approx. 5 %. A screening examination by an ophthalmologist is not mandatory in Germany.
Source: "Früherkennung von Sehstörungen bei Kindern" Michael Gräf in Deutsches Ärzteblatt, Jg.104, Heft 11, 16.03.2007
How to perform the Brückner Test
The following parameters are essential when performing the Brückner test:
- Darkened room
- The patient – in this case a toddler – is sitting on the mother’s/father’s lap
- The doctor looks through the ophthalmoscope, patient must fixate on the light of the ophthalmoscope
- Both eyes are illuminated with the ophthalmoscope simultaneously
- Distance between doctor and patient:
Depending on the distance, the test shows different sensitivity for different causes of amblyopia.
Therefore it is recommended to conduct the test from a close distance (0.2 to 1 m) as well as from a long distance (3 to 4 m).

Findings:
In normal cases, both pupils shine equally. Findings such as both pupils shine differently, punctuate lens opacities or diffuse lens clouding and leukokoria (white pupillary reflex) ought to be interpreted as pathological and require urgent ophthalmological examination.

The table shows which distances increase the sensitivity for certain eye disorders.

Comparison of normal finding and pathological finding at different examination distances
It is essential to perform the Brückner test at a close distance as well as at a long distance. At a close examination (10 to 20 cm) anisometropia and myopia can hardly be distinguished from the normal finding. (Picture 1, close examination, left column at the bottom). They can only be detected in an examination at a greater distance (4 m), as shown in the simulated pictures below. At an examination at distance (4 m) the examiner only concentrates on the brightness of both pupils and whether the red reflex is weaker in one or both pupils. The iris cannot be seen at this distance. If necessary, the comparison with the red reflex of a parent (also with glasses) of the child may be helpful. Please note: At a distance of 4 m, the darker pupil corresponds to the eye with the stronger ametropia. In the classic examination distance of 0.5 to 1 m however, the pupil with the stronger ametropic eye may shine brighter.
Illustration of findings of the transillumination test at a distance of 10 cm.
The small picture details show findings at a distance of 4 m.
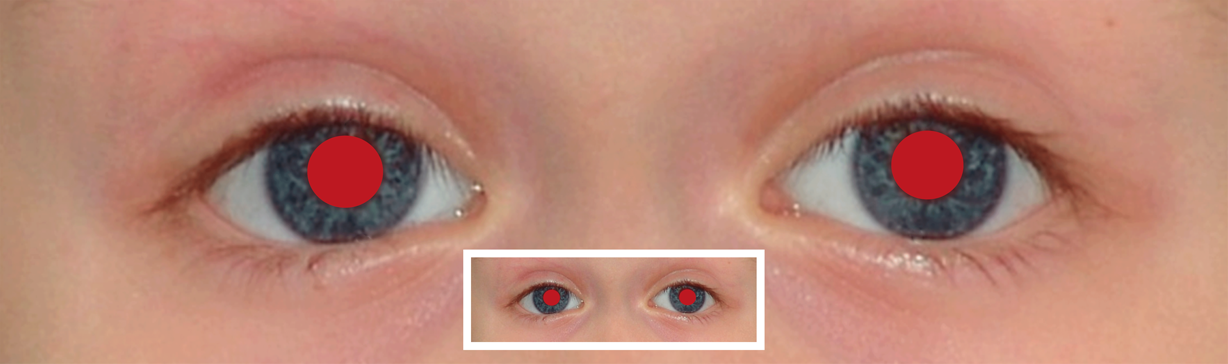
normal finding
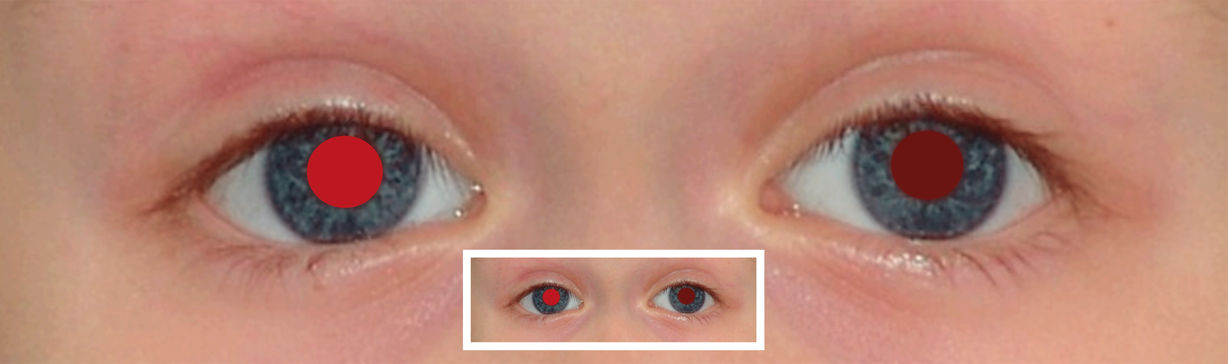
diffuse cataract
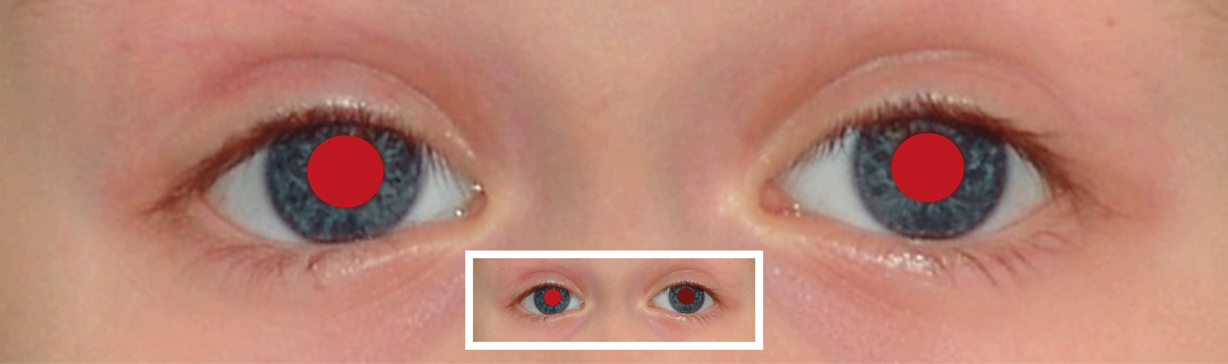
anisometropia
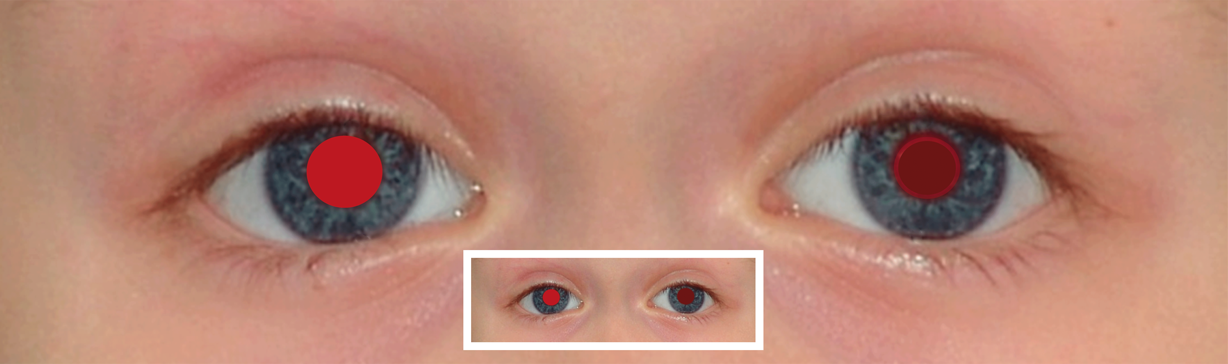
nucleus cataract
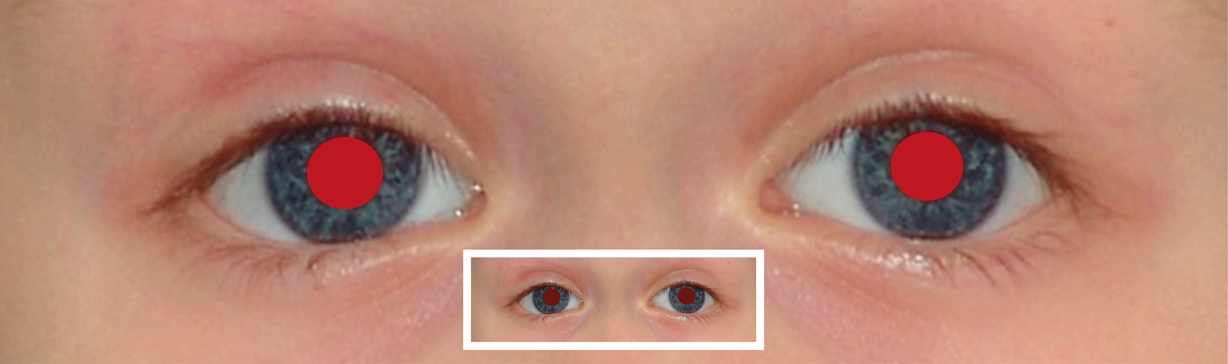
bilateral myopia/hyperopia

posterior polar cataract
Brückner test examination of a sleeping child
Opening the eye lids
The eye lids of a sleeping child can be opened by carefully spreading the lids with thumb and forefinger of your free hand and carefully lifting the upper lid with the thumb while e.g. the mother holds the lower lid with her finger. Avoid touching the conjunctiva and the eye. Folding of the lid can be prevented by gently pushing it against the eye.
To trigger the eye opening reflex, the mother, holding the baby upright between her hands and stabilizing its head, is moving the baby rhythmically up and down once a second on a distance of 30 cm. The resulting acceleration evokes the opening of the eyes, lifting of the eye brows and wrinkling of the baby’s forehead. For the examination, the movement is interrupted.
M Gräf in "The transillumination test according to Brücker“, Pediatric and Adolescent Medicine 3/2014 Schattauer

Safety for you and your patients
The use of light sources, such as conventional pocket lights, is often mistakenly seen as being harmless for eye examinations and requires urgent clarification.
Light can be a danger to the retina and the skin surface, depending on the intensity and the light source. Certain UV-A rays may be dangerous for the eye. Possible eye damages include conjunctivitis, blindness of the cornea and lens opacity. Negative skin effects include skin burns and loss of skin elasticity.
To be used as light source for the examination of eyes, a device has to be approved in accordance to the Act on Medical Devices and fulfil the requirements of relevant standards. For specific ophthalmic products the threshold value of DIN EN ISO 15004-2 applies.
Other medical products with light sources, such as otoscopes, have to fulfil the requirements for photo biological safety in accordance to DIN EN 62471 – these devices are however not approved for eye examinations.
Practitioners should be aware of possible irreversible damages as well as possible recourse claims.
HEINE is testing all of its products according to their intended application and therefore fulfils all relevant standards. Guaranteeing the safety of patients and the user is part of our high quality standard.
Studies and links
 | The Brückner testSource: Graefe's Archive for Clinical and Experimental Ophthalmology January 2008, Volume 246, Issue 1, pp 135-141;First online: 30 June 2007 |
 | Red Reflex Examination in Neonates, Infants, and ChildrenDecember 2008, VOLUME 122 / ISSUE 6 |
 | How to test for the red reflex in a childCommunity Eye Health 2014; 27(86): 36. |
How to conduct the Brückner test with a direct ophthalmoscope


The Rekoss Disc
The direct ophthalmoscope has a Rekoss disc, which allows switching on corrective lenses. They are used to compensate for refractive errors in both doctor and patient and help you to get a sharp examination image. Select the value which corresponds to the sum of the spherical refractive error of patient and examiner.
The setting of the Rekoss disc has to be changed depending on the distance between practitioner and patient during the Brückner test. An individual setting is also necessary for fundoscopy.
The following applies for the Brückner test: for distances of 4 m to 1 m without glasses select the dioptric power of your own eyeglasses. For less than 1 m, from the age of 40, rotate the Rekoss disc to the plus values to ensure you have a sharp image of the iris. Chose the large spot aperture for the Brückner test. For a close examination reduce the brightness (less disturbing reflexes, larger pupil).
The aperture wheel
Different apertures can be chosen on the back of the ophthalmoscope (patient side) such as fixation star, different spot sizes, hemispot and slit as well as red-free and blue filter.
Choosing the right aperture:
 | Small spot: provides easy view of the fundus through un undilated pupil. Always start the examination with this aperture and proceed to micro spot if pupil is particularly small and / or sensitive to light. |
 | Large spot: standard aperture for dilated pupil and general examination of the eye. |
 | Pinhole: allows easy entry into very small, undilated / miotic pupils. |
 | Slit: helpful in determining various elevations of lesions, particularly tumours and oedematous discs. |
 | Hemispot: provides a combination of the depth perception of the slit and the field of view of the large spot. |
 | Fixation star: allows the observation / assessment of eccentric fixation. |
 | Blue filter: used with fluorescein dye allows the identification of small lesions, abrasions and foreign objects. |
 | Red-free filter: allows an easy identification of vessels, arteries and nerve fibres. |
Direct Ophthalmoscopy – Funduscopy with the handheld ophthalmoscope
The direct ophthalmoscope allows the examination of the central fundus. Hold the ophthalmoscope very close in front of the patient’s eye. The patient directs his view to the ear of the practitioner. The practitioner uses his left eye for the examination of the left eye of the patient and his right eye for the examination of the patient’s right eye while looking through the ophthalmoscope at a very short working distance. During the examination of the left eye, the patient should look to the right ear of the examiner.
In order to get a sharp image, use the refractive compensation via the Rekoss disc. With the help of additional lenses refractive errors in both doctor and patient are compensated by adding the dioptre number.
Different apertures and filters can be selected on the aperture wheel at the back (patient side) of the ophthalmoscope, which offer various viewing options.
In a normal finding, the pupil is sharply defined, well pigmented and has a central, small excavation. By tilting the ophthalmoscope, other areas of the fundus can be examined. Retinal blood vessels show a normal calibre und are slightly tortuous.
The macula can be seen, if the patient looks directly into the ophthalmoscope. The fixation can be checked by using the fixation star aperture on the ophthalmoscope.
Video:
Watch this video for detailed information about direct ophthalmoscopy.
Which ophthalmoscope is best suited for your paediatrician practice?
HEINE offers the right ophthalmoscope for any demand – in highest quality. The “Aspherical Optical System” (AOS) from HEINE eliminates corneal and iris reflexes to provide large, crisp and glare-free fundus images. HEINE LED illumination has been engineered to provide optimal illumination which is ideally suited for the intended application.
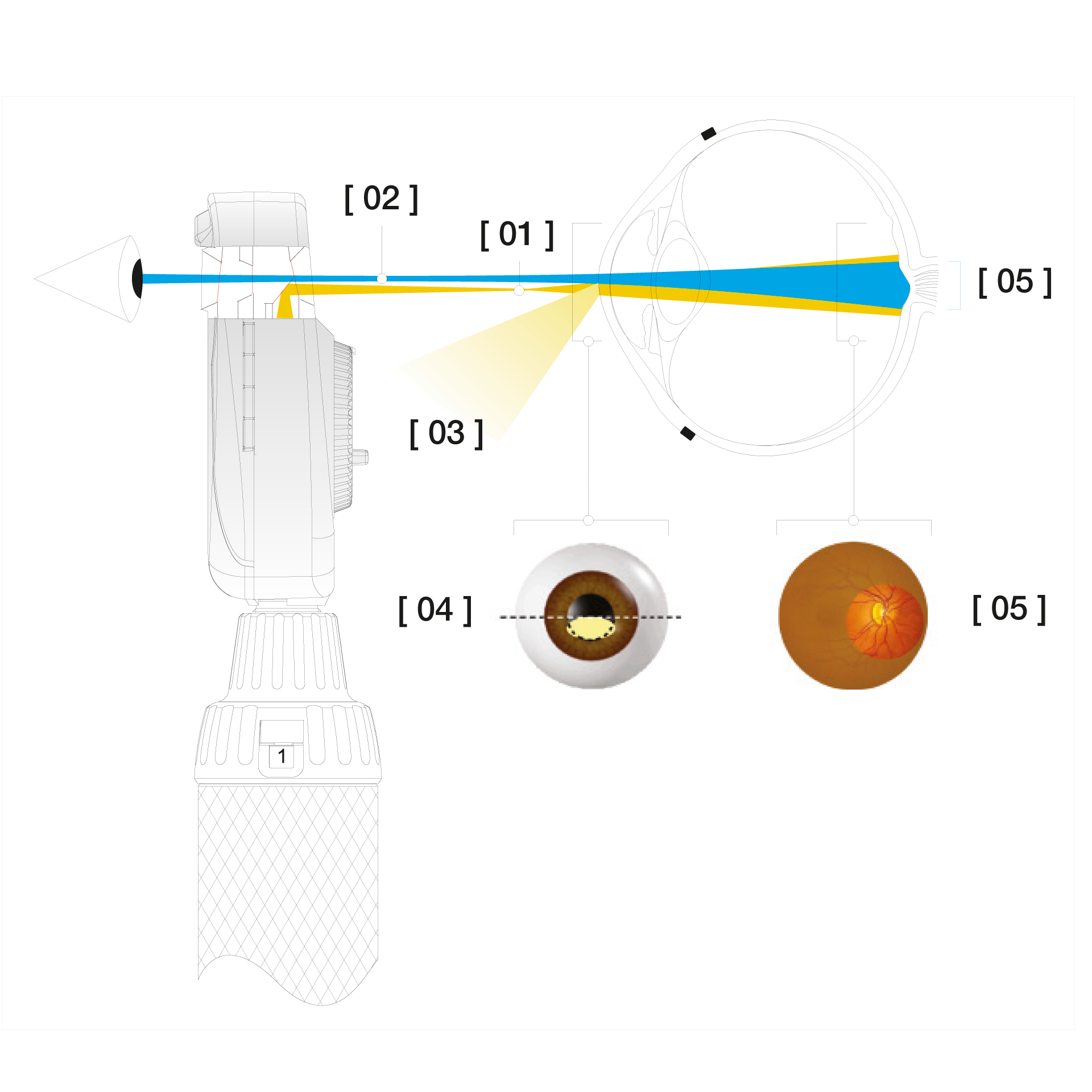
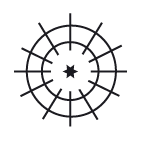
The Aspherical Optical System
[01] Flat, elliptical illumination beam produced by HEINE’s patented Aspherical Optical System.
[02] Observation path.
[03] Redirected iris and corneal reflexes.
[04] The elliptical light beam enters through the lower half of the cornea. The illumination beam has been separated from the observation beam (Gullstrand-Principle).
All reflexes are diverted away from the observation beam due to the curvature of the reflective cornea. Due to the flat, compressed form of the light beam, a maximum amount of light enters through the pupil.
[05] Once past the anterior chamber, the light beam opens up dramatically to illuminate a large area of the retina.
Our portfolio at a glance
We will be happy to advise you free of charge and without any obligation.
Please contact us here.



