Colour filters when using an indirect ophthalmoscope
Red-free, yellow and blue filter
Whatever the filter’s colour, when using the binocular indirect ophthalmoscope, you should use as little light as possible and as much light as necessary!
It’s best to start with a low light intensity at the beginning of the examination and to slowly increase it under visualisation with the loupe, enabling ideal examination with the best view of the retina and adequate patient comfort.

No filter / white light
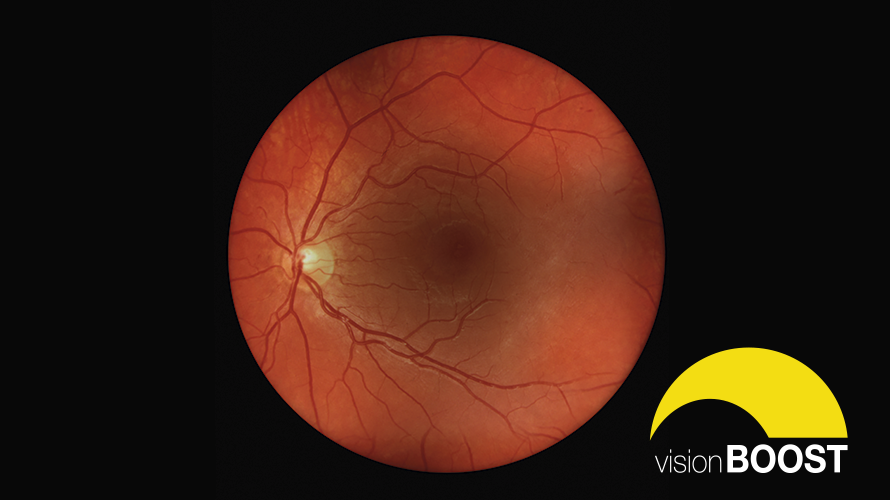
The fundus can be viewed in its natural hue and saturation with white light.
The white light is used as a standard light with its true colours at the start of the examination to get an overview.
Red-free filter (green colour)
The retina has a predominantly red hue when the fundus is examined with white light.
With the green light-producing filter, the longer wavelengths in the light’s red spectrum are blocked (making it red-free). This suppresses what is known as ‘visual noise’ and thus allows a clearer contrast between structures and the surrounding tissue.
Red-free light also provides a better view by suppressing scattering when the media in the illumination beam are cloudy – when there is a cataract, for example.
What’s more, defects in the retinal nerve’s fibre bundle can be detected far quicker and easier with this light filter. For example, damage to the fibre bundle can be reliably diagnosed in advanced glaucoma, and a glaucomatous cup-to-disc ratio in the optic nerve papilla is easier to assess since the structures contrast better.
This filter also allows for ideal examination of blood vessels (blood appears almost black in red-free light). Calibre and reflex irregularities, as well as crossover signs like those found in arterial hypertension, can be defined more clearly.
With the white light (no filter), it’s easy to overlook a small arterial branch occlusion that doesn’t show the typical red spot in the middle of the macula, especially if the oedema in the retinal nerve’s fibre layer isn’t very pronounced (yet). There’s usually no overlooking changes like this in the red-free light. However small and subtle it might be, the defined oedema jumps out at the examiner in the red-free light.
Green wavelengths don’t penetrate the choroid. This explains the well-known phenomenon that choroidal lesions seem to disappear when the red-free filter is applied.
So the filter is also used to make a distinction between retinal and choroidal naevi.
Yellow filter
The yellow filter can be described as a comfort filter for the patient and the examiner alike, since it reduces photophobia with its warm, soft light. Many practitioners use it on sensitive patients. It has a protective effect too by reducing UV exposure.
Blue filter
This filter is, quite unfairly, neglected by many users.
Blue light is reflected by the membrana limitans interna and the anterior retinal layers. So this filter is particularly suitable for distinguishing between pathologies in front of these layers, such as epiretinal or fibrovascular membranes like those encountered in proliferative diabetic retinopathy.
The blue filter is rarely used, but can be put to good use for the optic disc drusen. The drusen are easier to see here since the optic nerve papilla is more reflective, but not as much as in an autofluorescence image.
This colour filter can also be used to perform fluorescein angioscopy – the examination of the peripheral retina with a blue filter to identify peripheral neovascularisation once the patient has been administered sodium fluorescein intravenously. It is often difficult, or even impossible, to photographically document peripheral images during fluorescein angiography. But, with the indirect ophthalmoscope, the periphery can be scanned for vascularisation with a quick glance, which may be indicative of further treatment if there is suspicion of proliferative diabetic retinopathy or other pathologies.
visionBOOST
In the case of particularly dense and cloudy media, like an advanced cataract, the retina can often only be seen to a limited extent – if it’s even visible in the first place. Even the maximum brightness level doesn’t give an examiner a detailed view of the retina.
This is where visionBOOST, an exclusive feature of the HEINE OMEGA 600, comes into play. If the brightness control on the head-worn ophthalmoscope is turned slowly once it has stopped in the standard mode, the light intensity is increased beyond the usual level. This allows a brief, important view of the retina behind the opacity, even in the case of the densest media.
By Dr Vera Schmit-Eilenberger, ophthalmology specialist
More Information

The new high-end indirect ophthalmoscope

Brückner Test with the direct ophthalmoscope

Click here to read more about the visionBOOST