Alopecia areata
Alopecia areata is a harmless, non-infectious, inflammatory loss of hair that can affect adults and children of both genders at any time to varying degrees.
The trigger is unknown, but it is believed that this is an autoimmune disease with a genetic predisposition: 20–25 per cent of all affected individuals have a “related” autoimmune disease (e.g. Type I diabetes mellitus, Hashimoto thyroiditis, or vitiligo).
Diagnosis of alopecia areata
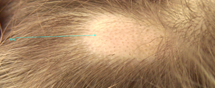
A dermatoscope is becoming increasingly more important in the diagnosis of alopecia areata. Performing a biopsy on the scalp of an already traumatised patient is not well tolerated! Furthermore, a dermatoscope also serves the therapeutic course and is suitable for distinguishing alopecia areata from scarring alopecia or alopecia mechanica.
When assessing a hairless area, one usually sees short vellus hair, curved “comma hair”, black points, empty follicular ostia, and yellow, punctate areas that occasionally enclose black points.
A dense lymphocytic perifollicular infiltrate with focal follicle infiltration can be seen in histological examinations. Interferon-gamma and interleukin 2 as well as interleukin-15 receptor B are involved in the pathogenesis. Only hair follicles in the growth phase (anagen phase) are affected. The infiltrate damages the hair follicle, thereby leading to dystrophy of the hair shaft and ultimately breakage, incomplete keratinisation, or hair loss and reduction to miniature follicles. The cyclic renewal of the hair follicle (catagen/telogen) is maintained, thereby leading to regression of the infiltrate. The new anagen phase then leads to either a renewed attack of infiltrate or spontaneous hair growth. Spontaneous regrowth usually occurs in the centre of the bald spot and spreads out to the periphery.
The prognosis depends on the extent and the number of bald areas as well as the duration. As a rule of thumb, within the first six months, approximately 30% of alopecia areata patients demonstrate renewed growth or complete healing.